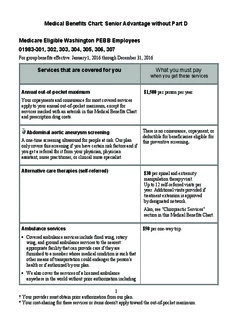
Table Of ContentMedical Benefits Chart: Senior Advantage without Part D
Medicare Eligible Washington PEBB Employees
01983-301, 302, 303, 304, 305, 306, 307
For group benefits effective: January 1, 2016 through December 31, 2016
Services that are covered for you What you must pay
when you get these services
Annual out-of-pocket maximum $1,500 per person per year.
Your copayments and coinsurance for most covered services
apply to your annual out-of-pocket maximum, except for
services marked with an asterisk in this Medical Benefits Chart
and prescription drug costs.
There is no coinsurance, copayment, or
Abdominal aortic aneurysm screening
deductible for beneficiaries eligible for
A one-time screening ultrasound for people at risk. Our plan
this preventive screening.
only covers this screening if you have certain risk factors and if
you get a referral for it from your physician, physician
assistant, nurse practitioner, or clinical nurse specialist.
Alternative care therapies (self-referred)
$30 per spinal and extremity
manipulation therapy visit.
Up to 12 self-referred visits per
year. Additional visits provided if
treatment extension is approved
by designated network.
Also, see "Chiropractic Services"
section in this Medical Benefits Chart.
Ambulance services $50 per one-way trip.
• Covered ambulance services include fixed wing, rotary
wing, and ground ambulance services to the nearest
appropriate facility that can provide care if they are
furnished to a member whose medical condition is such that
other means of transportation could endanger the person's
health or if authorized by our plan.
• We also cover the services of a licensed ambulance
anywhere in the world without prior authorization including
1
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
transportation through the 911 emergency response system
where available if one of the following is true:
♦ You reasonably believe that you have an emergency
medical condition and you reasonably believe that your
condition requires the clinical support of ambulance
transport services.
♦ Your treating physician determines that you must be
transported to another facility because your emergency
medical condition is not stabilized and the care you need
is not available at the treating facility.
♦ You may need to file a claim for reimbursement unless the
provider agrees to bill us (see Chapter 7).
• †Nonemergency transportation by ambulance is appropriate
if it is documented that the member's condition is such that
other means of transportation could endanger the person's
health and that transportation by ambulance is medically
required.
There is no coinsurance, copayment, or
Annual routine physical exams
deductible for this preventive care.
Routine physical exams are covered if the exam is medically
appropriate preventive care in accord with generally
accepted professional standards of practice. This exam is
covered once every 12 months.
There is no coinsurance, copayment,
Annual wellness visit
or deductible for the annual wellness
If you've had Part B for longer than 12 months, you can get an
visit.
annual wellness visit to develop or update a personalized
prevention plan based on your current health and risk factors.
This is covered once every 12 months.
Note: Your first annual wellness visit can't take place within
12 months of your "Welcome to Medicare" preventive visit.
However, you don't need to have had a "Welcome to
Medicare" visit to be covered for annual wellness visits after
you've had Part B for 12 months.
2
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
There is no coinsurance, copayment,
Bone mass measurement
or deductible for Medicare-covered
For qualified individuals (generally, this means people at
bone mass measurement.
risk of losing bone mass or at risk of osteoporosis), the
following services are covered every 24 months or more
frequently if medically necessary: procedures to identify
bone mass, detect bone loss, or determine bone quality,
including a physician's interpretation of the results.
There is no coinsurance, copayment, or
Breast cancer screening (mammograms)
deductible for covered screening
Covered services include:
mammograms.
• One baseline mammogram between the ages of 35 and 39.
• One screening mammogram every 12 months for women age
40 and older.
• Clinical breast exams once every 24 months.
Cardiac rehabilitation services† $30 per visit.
Comprehensive programs for cardiac rehabilitation services
that include exercise, education, and counseling are covered for
members who meet certain conditions with a doctor's order.
Our plan also covers intensive cardiac rehabilitation programs
that are typically more rigorous or more intense than cardiac
rehabilitation programs.
There is no coinsurance, copayment,
Cardiovascular disease risk reduction visit
or deductible for the intensive
(therapy for cardiovascular disease)
behavioral therapy cardiovascular
We cover one visit per year with your primary care doctor to
disease preventive benefit.
help lower your risk for cardiovascular disease. During this
visit, your doctor may discuss aspirin use (if appropriate),
check your blood pressure, and give you tips to make sure
you're eating well.
There is no coinsurance, copayment,
Cardiovascular disease testing
or deductible for cardiovascular
Blood tests for the detection of cardiovascular disease (or
disease testing that is covered once
abnormalities associated with an elevated risk of
every five years.
cardiovascular disease) once every five years (60 months).
3
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
There is no coinsurance, copayment,
Cervical and vaginal cancer screening
or deductible for Medicare-covered
Covered services include:
preventive Pap and pelvic exams.
• For all women: Pap tests and pelvic exams are covered once
every 24 months.
• If you are at high risk of cervical cancer or have had an
abnormal Pap test and are of childbearing age: one Pap test
every 12 months.
Chiropractic services† $20 per visit.
Covered services include:
• We cover only manual manipulation of the spine to correct
subluxation. These Medicare-covered services are provided
by a participating chiropractor of the CHP Group and listed
in the Senior Advantage Directory.
There is no coinsurance, copayment, or
Colorectal cancer screening
deductible for a Medicare-covered
• For people 50 and older, the following are covered: colorectal cancer screening exam.
♦ Flexible sigmoidoscopy (or screening barium enema as an
alternative) every 48 months.
♦ Fecal occult blood test, every 12 months.
• For people at high risk of colorectal cancer, we cover a
screening colonoscopy (or screening barium enema as an
alternative) every 24 months.
• For people not at high risk of colorectal cancer, we cover a
screening colonoscopy every 10 years (120 months), but not
within 48 months of a screening sigmoidoscopy.
4
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
Dependent Children Out-of-Area Coverage
A limited dependent children out-of-area benefit is available to
dependents who are temporarily outside our service area.
We make limited payments for medically necessary routine,
continuing, and follow-up medical care that a qualifying
20% of the actual fee the provider,
dependent receives from non-plan providers outside our service
facility, or vendor charges.
area, but inside the U.S. (which for the purpose of this benefit
means the 50 states, the District of Columbia, and U.S.
territories).
This dependent children out-of-area benefit cannot be
combined with any other benefit we are covering elsewhere
within this Medical Benefits Chart.
There is no coinsurance, copayment, or
Depression screening
deductible for an annual depression
We cover one screening for depression per year. The screening
screening visit.
must be done in a primary care setting that can provide follow-
up treatment and referrals.
There is no coinsurance, copayment, or
Diabetes screening
deductible for the Medicare-covered
We cover this screening (includes fasting glucose tests) if you
diabetes screening tests.
have any of the following risk factors: high blood pressure
(hypertension), history of abnormal cholesterol and triglyceride
levels (dyslipidemia), obesity, or a history of high blood sugar
(glucose). Tests may also be covered if you meet other
requirements, like being overweight and having a family
history of diabetes.
Based on the results of these tests, you may be eligible for up to
two diabetes screenings every 12 months.
Diabetes self-management training and diabetic No charge.
services and supplies
For all people who have diabetes (insulin and noninsulin users),
covered services include:
• †Supplies to monitor your blood glucose: Blood glucose
monitor, blood glucose test strips, lancet devices, lancets,
and glucose-control solutions for checking the accuracy of
test strips and monitors.
5
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
• †For people with diabetes who have severe diabetic foot No charge.
disease: One pair per calendar year of therapeutic custom-
molded shoes (including inserts provided with such shoes)
and two additional pairs of inserts, or one pair of depth shoes
and three pairs of inserts (not including the noncustomized
removable inserts provided with such shoes). Coverage
includes fitting.
• Diabetes self-management training is covered under There is no coinsurance, copayment, or
deductible for beneficiaries eligible for
certain conditions.
the diabetes self-management training
preventive benefit.
Durable medical equipment and related supplies†
No charge for each item when
(For a definition of "durable medical equipment," see Chapter provided within the service area.
10 of this booklet.)
No charge for certain items such as
Covered items include, but are not limited to: wheelchairs, home ventilators and home IV infusion
crutches, hospital bed, IV infusion pump, oxygen equipment, pump equipment and supplies.
nebulizer, and walker.
We cover all medically necessary durable medical equipment
covered by Original Medicare. If our supplier in your area does
not carry a particular brand or manufacturer, you may ask them
if they can special order it for you. The most recent list of
suppliers is available on our website at kp.org.
6
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
Emergency care $50 per emergency department visit.
Emergency care refers to services that are: This copayment does not apply if you
are immediately admitted directly to the
• Furnished by a provider qualified to furnish emergency
hospital as an inpatient (it does apply if
services, and
you are admitted as anything other than
• Needed to evaluate or stabilize an emergency medical an inpatient; for example, it does apply
condition. if you are admitted for observation).
A medical emergency is when you, or any other prudent †If you receive emergency care at an
layperson with an average knowledge of health and medicine, out-of-network hospital and need
believe that you have medical symptoms that require immediate inpatient care after your emergency
medical attention to prevent loss of life, loss of a limb, or loss condition is stabilized, you must return
of function of a limb. The medical symptoms may be an illness, to a network hospital in order for your
injury, severe pain, or a medical condition that is quickly care to continue to be covered or you
getting worse. must have your inpatient care at the
out-of-network hospital authorized by
You have worldwide emergency coverage.
our plan and your cost is the cost-
sharing you would pay at a network
hospital.
The amount you pay per class or
Health and wellness education programs
session varies depending upon the class
These are programs focused on health conditions such as high
or session, but you will not pay more
blood pressure, cholesterol, asthma, and special diets. Programs
than $120 per visit.
designed to enrich the health and lifestyles of members include
Newsletters and our nursing hotline are
weight management, fitness, and stress management.
provided at no charge.
Health education classes, nutritional training, and wellness
programs are listed in our health and wellness classes and
resources catalog, including the cost-sharing for each class or
session. Contact Member Services for more details or for a
copy of the health and wellness classes and resources catalog.
Hearing services $30 per office visit.
• Diagnostic hearing and balance evaluations performed by
your provider to determine if you need medical treatment are
covered as outpatient care when furnished by a physician,
audiologist, or other qualified provider.
• Routine hearing exams.
7
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
• Hearing aids. Benefit allowance maximum of up to
$800 every 36 months.
(If covered, see rider document in the
EOC for additional information.)
There is no coinsurance, copayment, or
HIV screening
deductible for beneficiaries eligible for
• For people who ask for an HIV screening test or who are at Medicare-covered preventive HIV
increased risk for HIV infection, we cover one screening
screening.
exam every 12 months.
• For women who are pregnant, we cover up to three screening
exams during a pregnancy.
• HIV screening test after each exposure. No charge.
Home health agency care† No charge.
Prior to receiving home health services, a doctor must certify Note: There is no cost-sharing for
that you need home health services and will order home health home health care services and items
services to be provided by a home health agency. You must be provided in accord with Medicare
homebound, which means leaving home is a major effort. guidelines. However, the applicable
cost-sharing listed elsewhere in this
Covered services include, but are not limited to:
Medical Benefits Chart will apply if the
• Part-time or intermittent skilled nursing and home health item is covered under a different
aide services. To be covered under the home health care benefit; for example, durable medical
benefit, your skilled nursing and home health aide services equipment not provided by a home
combined must total fewer than 8 hours per day and 35 hours health agency.
per week.
• Physical therapy, occupational therapy, and speech therapy.
• Medical and social services.
• Medical equipment and supplies.
Home infusion therapy† No charge.
We cover home infusion supplies and drugs if all of the
following are true:
• Your prescription drug is on our standard formulary (or you
have a formulary exception).
8
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
• We approved your prescription drug for home infusion
therapy.
• Your prescription is written by a network provider and filled
at a network home-infusion pharmacy.
Hospice care When you enroll in a Medicare-
certified hospice program, your hospice
You may receive care from any Medicare-certified hospice
services and your Part A and Part B
program. You are eligible for the hospice benefit when your
services related to your terminal
doctor and the hospice medical director have given you a
prognosis are paid for by Original
terminal prognosis certifying that you're terminally ill and have
Medicare, not our plan.
six months or less to live if your illness runs its normal course.
Your hospice doctor can be a network provider or an out-of-
network provider.
Covered services include:
• Drugs for symptom control and pain relief.
• Short-term respite care.
• Home care.
*For hospice services and services that are covered by
Medicare Part A or B and are related to your terminal
prognosis: Original Medicare (rather than our plan) will pay
for your hospice services and any Part A and Part B services
related to your terminal prognosis. While you are in the hospice
program, your hospice provider will bill Original Medicare for
the services that Original Medicare pays for.
For services that are covered by Medicare Part A or B and
are not related to your terminal prognosis: If you need
nonemergency, non–urgently needed services that are covered
under Medicare Part A or B and that are not related to your
terminal prognosis, your cost for these services depends on
whether you use a provider in our plan's network:
• If you obtain the covered services from a network provider,
you only pay the plan cost-sharing amount for in-network
services.
• *If you obtain the covered services from an out-of-network
provider, you pay the cost-sharing under Fee-for-Service
Medicare (Original Medicare).
9
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Services that are covered for you What you must pay
when you get these services
For services that are covered by our plan but are not
covered by Medicare Part A or B: We will continue to cover
plan-covered services that are not covered under Part A or B
whether or not they are related to your terminal prognosis. You
pay your plan cost-sharing amount for these services.
Note: If you need nonhospice care (care that is not related to
your terminal prognosis), you should contact us to arrange the
services. Getting your nonhospice care through our network
providers will lower your share of the costs for the services.
Our plan covers hospice consultation services (one time only) No charge.
for a terminally ill person who hasn't elected the hospice
benefit.
There is no coinsurance, copayment, or
Immunizations
deductible for the pneumonia,
Covered Medicare Part B services include:
influenza, and Hepatitis B vaccines.
• Pneumonia vaccine.
• Flu shots, once a year in the fall or winter.
• Hepatitis B vaccine if you are at high or intermediate risk of
getting Hepatitis B.
• Other vaccines if you are at risk and they meet Medicare Part
B coverage rules.
Inpatient hospital care† Cost-sharing is charged for each
inpatient stay.
Includes inpatient acute, inpatient rehabilitation, long-term care
hospitals, and other types of inpatient hospital services. $500 per admission.
Inpatient hospital care starts the day you are formally admitted
Thereafter there is no charge for the
to the hospital with a doctor's order. The day before you are
remainder of your covered hospital
discharged is your last inpatient day.
stay.
There is no limit to the number of medically necessary hospital
†If you get authorized inpatient care at
days or services that are generally and customarily provided by
an out-of-network hospital after your
acute care general hospitals. Covered services include, but are
emergency condition is stabilized, your
not limited to:
cost is the cost-sharing you would pay
• Semiprivate room (or a private room if medically necessary). at a network hospital.
• Meals, including special diets. Note: If you are admitted to the
hospital in 2015 and are not discharged
• Regular nursing services.
until sometime in 2016, the 2015 cost-
10
† Your provider must obtain prior authorization from our plan.
* Your cost-sharing for these services or items doesn't apply toward the out-of-pocket maximum.
Description:suppliers is available on our website at kp.org. No charge $800 every 36 months. For women who are pregnant, we cover up to three screening.